Well hey there, you’re back! Which tells me you’re not sick of this series I’ve been doing on my youngest. (No idea what’s going on? That’s ok! Check out parts 1, 2, and 3 here to get caught up.) For now, I think I’ve mostly given a high level update from birth through about ten months old. In this post, I’ll continue to share our toddler’s journey with hypotonia and the process to diagnosing or ruling out any causes of the delays in her gross motor development.

Originally we said we’d look at Olivia’s progress in therapy and see if a neurology consult was necessary at her 15 month well check. But at 11 months when the pediatrician called us in for a progress update, he spent a long time talking and observing Olivia and said he sees what we all see. In his words, he wasn’t comfortable with her fine and gross motor skills (or rather, lack thereof)—by then she should have been doing a lot more than she was, and he agreed that she had some asymmetry going on. You could tell more in person, but hopefully you can see it here in some of the pictures—her shoulders and her back and her legs are unevenly extended. She did not extend her right arm fully. Her right foot over rotates compared to her left. She was making some progress in PT with regard to gross motor, but since she still couldn’t get into/out of a seated position and could not roll on her own, let alone crawl, we wanted to go ahead and move her up for further evaluation. We expected her to be able to sit, pull up, roll after 7 weeks in PT and she wasn’t there yet.

The pediatrician didn’t specifically mention hypotonia that day, but we had talked about her lack of muscle tone previously. We weren’t sure if she just needed the nudge of physical therapy to get her going, or if perhaps there was another underlying cause at play. At this point in her journey she had begun OT (occupational therapy) for sensory defensiveness (some of her behaviors or lack of behaviors indicated a fine motor delay or sensory/tactile sensitivity). OT is a really nice bridge between PT and SLP (speech/language pathology, which is where she goes for feeding therapy). We were happy with her progress in feeding therapy with regard to her interest in self-feeding, and oral motor development. She had begun saying “dada” very excitedly whenever Jason walked into the room, so that was very encouraging.
Typically the things we would use to measure social/intellectual milestones at 11 months of age were things she could not do a result of her low muscle tone and poor motor coordination: babbling/words, self feeding, pointing or signing, nursery games like pat a cake, etc. Since at the time she couldn’t do them, it became hard to know if it was just muscle tone in her hands/arms/tongue causing the delay or something more. She was very engaging, though; she made eye contact, knew her name, made a lot of noise to communicate her needs (“chatty” with coos like a 4-6m old baby would be), responded with excitement or displeasure when familiar people come or go, etc.
Without waiting any longer, Olivia was referred to a pediatric neurologist. They have a developmental pediatrician as well (the idea was that regardless of neurological consult/eval results, our next step would be developmental pediatrics to make sure there’s nothing we’re overlooking). Olivia was delightfully cognitively/socially on target, but we were trying to figure out what, if anything, is causing her physical delays.

She was referred and seen quickly by a neurologist who referred her within a matter of days for an MRI, urine testing, and blood testing. They weren’t concerned that she’d never walk or that she’d had a stroke or anything, but they were curious to see what her brain looked like, and the testing could rule out any genetic anomalies or dietary causes that would coincide or cause the delays. Since she would need to be sedated for the MRI, we figured that was a good time to get the other tests done too (honest question: how ELSE do you get a urine sample on a very wiggly and floppy 11 month old who can’t sit by herself?). So on March 1, very very early in the morning, I had to NOT nurse my not-yet-sleeping-through-the-night baby and instead take her to the hospital. We had to be there for check-in an hour before her appt, which was at 7am! (If you know me, you know I am not a morning person).

They put her in the tiniest little gown I’ve ever seen, and we waaaaaaaaaited. I had pumped and brought a bottle along, just because I wasn’t sure what her mood was going to be like and I didn’t know what the nurses or I would need after. We ended up having to call the on-call doctor at the neurologist’s office because some of the specialized blood tests they ordered weren’t on her hospital order, and they almost didn’t do them! They had to call a pediatric team down to her bed to help attach the urine collection bag—nothing like making a big show wherever we go.

Because of the covid precautions in place, I was allowed in the waiting room but not in the test or exam room, so I had to hand off my little Squish when it was her time and head back out to the main hospital waiting room. After about an hour they called me back to the recovery room. She was having such a hard time waking up; she would whimper and fuss with her eyes closed, and she was extra wiggly and floppier than normal. She still had a specimen bag attached under the diaper, and that adorable little gown on. I couldn’t even deal with how cute she looked; I know that probably makes me sound like such a weirdo (and of course my tired selfies don’t do either of us justice)!
When she heard my voice, she started to perk up. After another 30 minutes of holding her and talking to her, she was much more awake but her throat was so dry (her little whimper was pathetic). I could tell she wanted milk but she couldn’t nurse, so I was thankful I’d brought that bottle along! She took it no problem, we confirmed the team got all the samples of urine and blood they needed, and we headed home to wait for results.
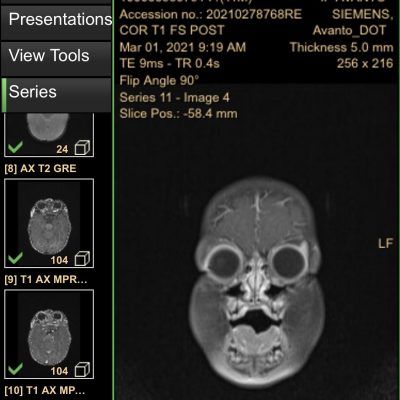
It took several weeks, but just in time for her 12 month well-check, we got her results. Her urine and amino acid tests and all the genetic tests were normal. Her MRI showed bilateral diffusivity in the central tegmental tracts. (Say that three times fast!) What do those words even mean? Goooooooood question. Apparently, some of the white spots they saw with the contrast on her MRI can be seen in normal cases, but can also be seen in the brains of children with certain seizure disorders. However, since she doesn’t appear to be having (or have had) any seizures, we’re taking that as “normal,” and that’s a good thing!
After that, things followed the status quo. She had her 1 year checkup, and we praised the progress of her therapies. The doctor mentioned her muscle tone was still low, but she met some huge milestones on her birthday: she got into and out of a seated position all on her own! That was huge, and the night after her birthday we finally were able to lower her crib for the first time since she was born. She started crawling soon after, and we continued to see continued forward progress (albeit slow at times) in gross motor, fine motor, feeding, and oral motor areas.
That’s it for now — stay tuned for the rest of the journey in the next post!