I recently wrote about Olivia’s birth story, our third girl born at the beginning of the pandemic. Since then, I’ve written a lot but never published the story of discovering her developmental delays and the adventure of her therapies (well, actually, I’ve posted about it on Instagram, but I’ve never blogged about it).
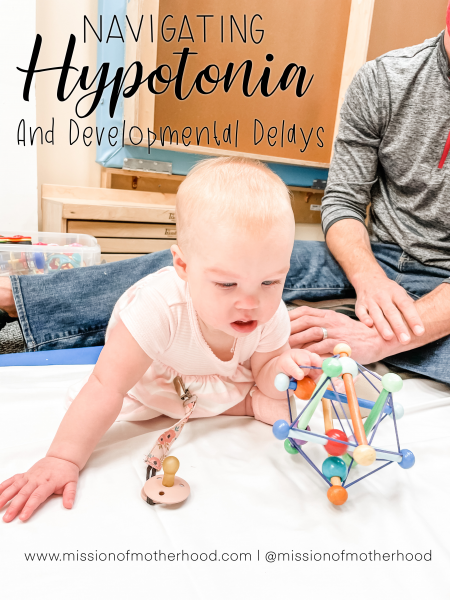
In December 2020 I took her for her 9 month well check. Using the ASQ-3 9-month form sent by her pediatrician, I confirmed several hunches that I’d had up to that point that she was not meeting milestones she should have been. She was referred for physical therapy to help her roll, get to sitting, and so on. At her visit, the pediatrician agreed that her growth and cognition were good, but that developmentally she seemed like she was at about 6 months.
We began PT right away. About a month in, we saw the pediatrician again to check progress and learned she likely has what’s called hypotonia (low muscle tone), but the level of severity is yet to be determined. For now, we think (and are hopeful!) it’s just mild. There can be some 600 causes, but if there’s no known cause, it’s called benign congenital hypotonia. It’s good to have the affirmation, get information, and start her therapies early. Instead of just a couple weeks of PT, she will likely be in it for a long haul. Muscle tone does not really change, but it’s different than strength. She also quickly began OT (occupational therapy for fine motor and life skills) and speech / feeding therapy soon after.
Most notably, hypotonia causes delayed gross motor development so she may just take longer to crawl and walk, depending on the severity— though that might be it. We learned she would eventually need orthotics as well (and they’re super cute), depending on progression and severity, which we would know in a few months. Adults with BCH can lead a relatively normal life especially in mild cases. A child with benign congenital hypotonia may not need any therapy, although they may need to see a doctor for related problems, such as joint dislocation.
Here’s a helpful link where you can read more about it, if you’re curious: https://surestep.net/blog/low-muscle-tone-hypotonia-an-overview-for-parents/. (A lot of my knowledge and what we’ve shared with our families is from that article, so SureStep folks, I’m not plagiarizing—you just said it best!) For a long time we heard from a lot of people that she was “fine,” or “just liked being held,” or would “do things in her own time.” It was hard in the throes of a pandemic for those who could not lay hands on her to grasp what we were experiencing.
When she was six weeks old she had a barium enema to rule out Hirschsprung’s disease because of some of her G.I. symptoms/behaviors, but thankfully it all came back normal. When I was reading about hypotonia, it was actually one of the things to rule out first (the symptoms in neonates can be very similar). Between that, her latch issues as a newborn, the “tough case” she was for the chiropractor post-frenectomy, and all of the behaviors that we observed at the speech and language pathologist when she was a few weeks old—it’s all coming together now and makes a ton of sense (it’s really interesting to look at her history up to this point).
When she was almost 10 months old, she was not sitting up or rolling over on her own, she was really poor at self-feeding, struggled to swallow even smooth purées, and couldn’t do much in the way of nursery games other than clapping. She couldn’t really sign or even babble words, etc. She was very floppy when held (or could not hold on), could not easily play with both hands, didn’t cross her midline or switch planes (think of forward reach as one plane and side reach as another plane, but she doesn’t rotate between the two). We’d never had to lower her crib mattress down from the newborn height because she couldn’t roll/ sit/pull up/cruise, etc. I had suspected since she was about a week old that something was just “off,” but because BCH primarily affects gross motor, it was tough to pin point until these bigger milestones were not being met. Rather than be upset that she was diagnosed with delays, I found myself feeling validated in a sobering way; obviously you don’t want your kid to have any needs or conditions that are going to potentially make things harder for them down the road.

I definitely believe early intervention is best so I’m very glad that we started PT immediately. I am also glad that the pediatrician validated my concerns and referred her right away. I did sort of start to spiral a little bit when I was reading about some of the things that kids with benign congenital hypotonia can need going forward (and of course the correlation among children with autism spectrum disorders), but ultimately I had to talk myself down off that ledge because we just aren’t there yet! I can’t fret about what school-age Olivia will need because school-age Olivia is future Caitlin‘s problem, you know?!
The long and short of it is she’s a sweet, smart, happy baby (BCH doesn’t affect kids cognitively, but it can affect their speech or when they talk because of the lack of muscle tone throughout their body, which includes in the tongue and mouth), and it’s possible all it means is that she will crawl and walk much later than her peers, and that might just be it! But as a result, she needs more physical attention because she’s frustrated that she can’t communicate or get where she’s going. We don’t feel blindsided by a diagnosis, but we also know God isn’t surprised. He’s gone before us, and we know He can be trusted!
“Treatment begins with a thorough diagnostic evaluation, usually performed by a neurologist, including an assessment of motor and sensory skills, balance and coordination, mental status, reflexes, and functioning of the nerves. Diagnostic tests that may be helpful include a CT or MRI scan of the brain, an EMG to evaluate nerve and muscle function, or an EEG to measure electrical activity in the brain. Once a diagnosis has been made, the underlying condition is treated first, followed by symptomatic and supportive therapy for the hypotonia. Physical therapy can improve motor control and overall body strength. Occupational therapy can help relearn ways to address activities of daily living. Speech-language therapy can help breathing, speech, and swallowing difficulties. Therapy for infants and young children may also include sensory stimulation programs.” (From NIH)
That’s the nutshell of the first update we sent to our families. I’ll publish these in a series so as not to overwhelm your inbox. Thanks for reading—and as always, feel free to leave a comment below with questions or support!



I found this blog last night when I couldn’t sleep. I brought my daughter home from India early December she is 20 months old through adoption. Last month she was diagnosed with hypotonia. It has been a whirlwind for me. I am Now advocating and getting the services that she needs. I am glad I came across this last night
So glad I could be of service to you! I sent you an email — I know it’s been a while but I would love to hear how you’re feeling now after a few months of advocating for her!